Breaking Up is Hard to Do – The sticky, icky world of biofilms
- Alia Khan-Elhady

- Jan 15, 2025
- 5 min read
Updated: Jan 16, 2025
Have you ever struggled to clean that slippery film off rocks in a creek or scrub away the slime from your dog’s water bowl? That slimy buildup is called a biofilm—a stubborn, sticky layer where microorganisms thrive.
Biofilms are bad for your health!
In the context of women’s pelvic health, biofilms play a major role in recurring urinary tract infections (UTIs) and other chronic conditions. Biofilms can form on the mucous membranes of the urinary tract, acting as an "invisibility cloak" for bacteria, particularly UTI-causing strains like E. coli. These bacterial colonies secrete a protective extracellular polymeric substance (EPS), making them resistant to antibiotics and immune defenses. This resilience contributes to persistent infections, reinfection cycles, and inflammation in the urinary and pelvic systems.
Biofilms can also be found on the skin, mucous membranes throughout the body, and on implanted medical devices. When they form it is difficult for your own immune defenses or antibiotic therapies to remove them. This can result in an ongoing cycle of health issues. Recurrent UTIs, tonsillitis, sinusitis, and GI issues are some examples.
In the last few decades, biofilms have been receiving more attention for the major role they play in ongoing conditions. In fact, the National Institutes of Health (NIH) revealed that 80% of chronic infections are associated with biofilm formation.1
Why are biofilms such a problem? Simply put, they are difficult to eradicate.
To better understand, let’s explore more about what biofilms are.
Biofilms: When Microorganisms Stick Together
We could actually learn a lot from biofilms.
They are living communities of organisms that stick together and attach to surfaces. Biofilms develop as a defense mechanism to prevent the clearance of undesirable microorganisms. They don’t discriminate. Bacterial, fungal, and viral species of microorganisms are all welcome to join this polymicrobial colony. And if speed is a virtue, they’ve got that covered. Biofilms can form in less than an hour.2
How do they form?
Biofilms are drastically different from free-floating microorganisms. Approximately 10% of bacteria are free-floating while the remaining 90% form colonies, excreting a sticky matrix called extracellular polymeric substance (EPS).3 The EPS creates a barrier protecting the internal microorganisms from the immune system and antimicrobials. Think of it as an invisibility cloak.
Once formed, the tight-knit community of microorganisms in a biofilm exchanges nutrients and ushers out waste. This creates an environment where a variety of microbial species can support each other and multiply.
Lifecycle of a Biofilm
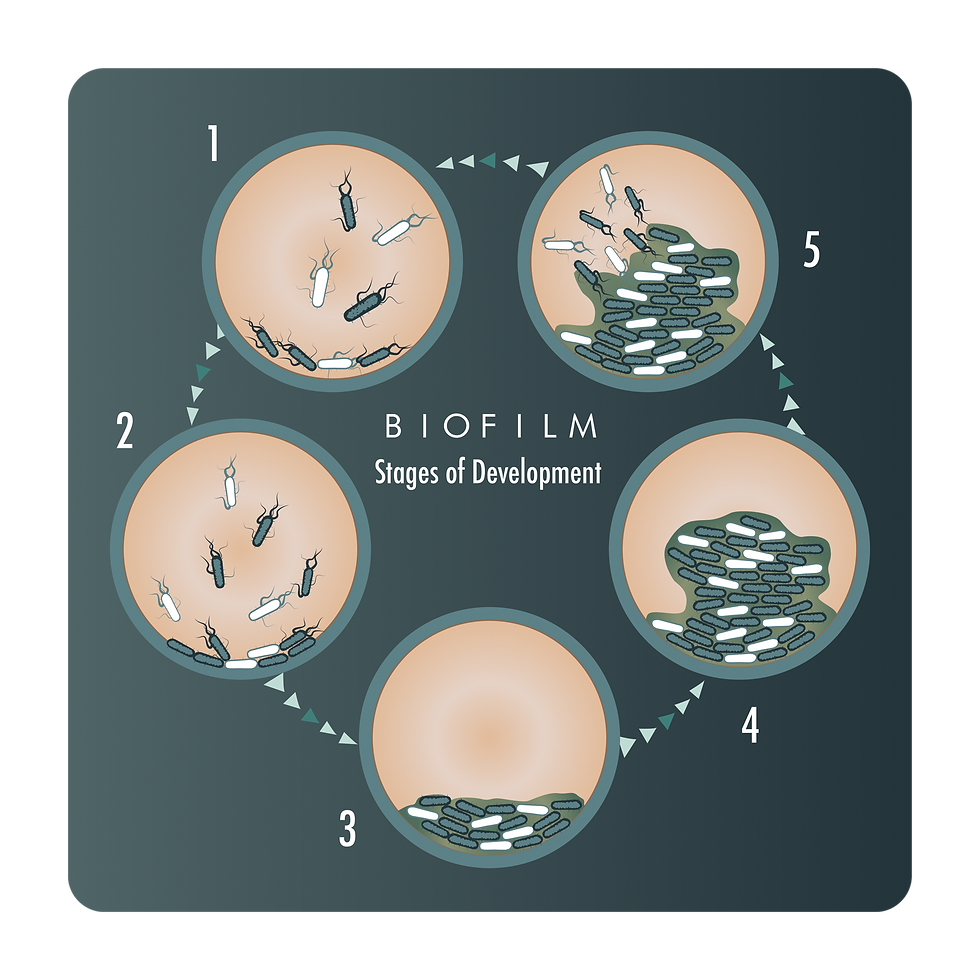
The lifecycle of a biofilm can be divided into five stages:
Initial Attachment – The formation begins with a reversible attachment of the free-floating microorganisms onto a surface.
Irreversible Attachment – The bacteria then form a single layer and irreversibly attach to tissues.
Maturation I – Formation of microcolonies through cell-to-cell communication. Colonies grow, multilayers appear, divide, and develop a biofilm.
Maturation II – During later stages, the biofilm forms a three-dimensional “mushroom”-like structure.
Dispersion – Finally, some cells start to detach and the biofilm will disperse, potentially reseeding infection and starting a new cycle of biofilm formation. This is the stage where individuals may experience a resurgence of problematic symptoms.
A hideout for the bad guys
By adopting an immobile mode of life embedded in a biofilm, harmful microorganisms enjoy several advantages over their free-floating counterparts:
Protection from environmental fluctuations in moisture, temperature, pH, and UV light
Capturing and concentrating environmental nutrients
Being shielded from host defense mechanisms – the EPS matrix acts like a force field and it is too large to be engulfed by immune cells
Antibiotic resistance – biofilm bacteria can resist up to 5000 times the antibiotic concentration that would normally be needed to resolve an infection4
In the last stage of development, dispersion, some cells of the mature biofilm start to detach and disperse into the environment as free-floating cells. During the dispersion stage, negative symptoms often resurface while the free-floating cells travel to other areas of the body to form a new biofilm and reseed infections.
Why are biofilms such a problem for UTIs?
Once biofilms form in the urinary tract, they become difficult to remove. The bacteria within exchange nutrients and resist being flushed out, making it easier for them to multiply and thrive. Studies have shown that biofilms contribute to as much as 80% of chronic infections, including recurrent UTIs.
How to stop the cycle?
Biofilms – with their ability to resist antibiotics and antimicrobial agents – create a barrier to optimal health. The treatment of biofilm-associated conditions is complicated. Fortunately,
ProVital Pharma's UROcomplex targets biofilms with a potent blend of science-backed ingredients. EGCG from green tea extract disrupts the biofilm matrix, while zinc bisglycinate and Vitamin C enhance the immune response and weaken bacterial defenses. The 100% bioavailable PACs and d-mannose block bacteria from adhering to the urinary tract, aiding in their removal. This multi-faceted approach breaks down biofilms, flushes out harmful bacteria, and prevents reinfection, restoring balance and promoting long-term urinary health.
How UROcomplex (Biophenol) Helps Break the CycleProVital Pharma’s UROcomplex directly addresses biofilm-related issues with a multi-pronged, science-backed approach:
Disruption of Biofilm Matrix: EGCG from green tea extract penetrates and destabilizes the biofilm structure, weakening its protective barrier.
Bacterial Anti-Adhesion: 100% bioavailable PACs and d-mannose prevent bacteria from attaching to the urinary tract lining, flushing them out during urination.
Immune Support: Zinc bisglycinate and Vitamin C bolster your immune defenses, enhancing your body's ability to clear bacterial invaders.
Microbiome Balance: Probiotics and prebiotics help restore the vaginal and gut microbiomes, reducing the likelihood of bacterial overgrowth and future biofilm formation.
By breaking down existing biofilms, preventing new ones from forming, and supporting overall pelvic health, UROcomplex helps women regain control, reducing the recurrence of UTIs and promoting lasting wellness.
Understanding biofilms – what they are, how they form, and how they impact health – is especially important for people who experience conditions that just won’t go away. Is that you? Perhaps it’s time to talk to your healthcare professional about whether biofilms might play a role and how you might start the UROcomplex regimen!
References:
Joo, H. S., & Otto, M. (2012). Molecular basis of in vivo biofilm formation by bacterial pathogens. Chemistry & biology, 19(12), 1503–1513. https://doi.org/10.1016/j.chembiol.2012.10.022
Hall-Stoodley L, Stoodley P. Biofilm formation and dispersal and the transmission of human pathogens. Trends Microbiol. 2005 Jan;13(1):7-10. doi: 10.1016/j.tim.2004.11.004.
Petrova, O. E., & Sauer, K. (2012). Sticky situations: key components that control bacterial surface attachment. Journal of bacteriology, 194(10), 2413–2425. https://doi.org/10.1128/JB.00003-12
Written by Alia Khan-Elhady, MSW, FNTP
Alia is Biocidin Botanicals' Lead Clinical Consultant. A licensed Social Worker and certified Functional Nutritional Therapist, she brings 15+ years of clinical experience to her role. Fueled by her own health journey, Alia is passionate about microbial balance and getting to the root cause of complex cases. She lives in Calgary, Canada, where she enjoys cooking whole foods from various cultures, inspired by her extensive travels.



Comments